|
Overview
 The human foot is a complex structure that absorbs shock every time we take a step. The foot has to adapt to a variety of movements during different forms of activities such as walking, running and climbing steps. The foot is made up of many different joints, ligaments and muscles which have to work together to allow us to move and balance. The arch of the foot plays and important role in absorbing shock and preventing over stressing of the foot muscles and bones. In this article, we shall briefly discuss flat feet and fallen arches. These two conditions are closely related to each other and can increase the risk of overuse injury to the foot. They can also cause overload of more proximal structures such as ankles, shins, knees and the lower back. Causes There are many different causes of flat feet, which can be separated into two main categories. The first category, congenital flat foot, is a condition that one is born with or is predisposed to at birth. This type includes the completely asymptomatic, pediatric flexible flat foot-by far the most common form of congenital flat foot. Flexible means that an arch is present until weight is put on the foot, at which time the arch disappears. This foot type is a result of the fact that all people are born with different physical features. Some people have bigger noses than others, just as some people have flatter feet (of course, there is no known correlation between the two). Any alteration in the many building blocks of the foot can influence its shape. At the other end of the spectrum, yet within the same category of congenital flat foot, exist several rare, more severe forms of flat foot. These severe conditions include Vertical Talus, Congenital Calcaneal Valgus, and Tarsal Coalitions - all of which are more rigid (no arch with or without weight on the foot) and definitely symptomatic. Luckily, these are much less common, but can usually be identified by specialists at the time of presentation and treated appropriately. The second category, acquired flat foot, develops over time, rather than at birth. Many different factors can contribute to the development of flat feet. These include the types of shoes a child wears, a child's sitting or sleeping positions, compensation for other abnormalities further up the leg, or more severe factors such as rupture of ligaments or tendons in the foot. Very commonly, the reason for flat feet is that the foot is compensating for a tight Achilles tendon. If the Achilles tendon is tight, then it causes the foot to point down, or to plantarflex (as occurs when stepping on the accelerator of your car). Even minimal amounts of plantarflexion can simulate a longer leg on that particular side, assuming that the other foot is in the normal position. The body therefore tries to compensate by pronating, or flattening out the arch, thereby making up for the perceived extra length on the affected side. Symptoms Flat feet don't usually cause problems, but they can put a strain on your muscles and ligaments (ligaments link two bones together at a joint). This may cause pain in your legs when you walk. If you have flat feet, you may experience pain in any of the following areas, the inside of your ankle, the arch of your foot, the outer side of your foot, the calf, the knee, hip or back. Some people with flat feet find that their weight is distributed unevenly, particularly if their foot rolls inwards too much (overpronates). If your foot overpronates, your shoes are likely to wear out quickly. Overpronation can also damage your ankle joint and Achilles tendon (the large tendon at the back of your ankle). Diagnosis People who have flat feet without signs or symptoms that bother them do not generally have to see a doctor or podiatrist about them. However, if any of the following occur, you should see your GP or a podiatrist. The fallen arches (flat feet) have developed recently. You experience pain in your feet, ankles or lower limbs. Your unpleasant symptoms do not improve with supportive, well-fitted shoes. Either or both feet are becoming flatter. Your feet feel rigid (stiff). Your feet feel heavy and unwieldy. Most qualified health care professionals can diagnose flat feet just by watching the patient stand, walk and examining his/her feet. A doctor will also look at the patient's medical history. The feet will be observed from the front and back. The patient may be asked to stand on tip-toe while the doctor examines the shape and functioning of each foot. In some cases the physician may order an X-ray, CT (computed tomography) scan, or MRI (magnetic resonance imaging) scan. high arch feet Non Surgical Treatment If you have flat feet, you may also experience pain throughout the lower body and into the lower back. Orthotics (custom-made rigid foot supports) can be prescribed when over-the-counter supports do not provide releif and surgery can also offer a more permanent solution in severe cases. The board-certified doctors in our practice would be able to select the most appropriate course of action in each case. Surgical Treatment  Feet that do not respond to the treatments above may need surgery. The surgery will help to create a supportive arch. After Care Patients may go home the day of surgery or they may require an overnight hospital stay. The leg will be placed in a splint or cast and should be kept elevated for the first two weeks. At that point, sutures are removed. A new cast or a removable boot is then placed. It is important that patients do not put any weight on the corrected foot for six to eight weeks following the operation. Patients may begin bearing weight at eight weeks and usually progress to full weightbearing by 10 to 12 weeks. For some patients, weightbearing requires additional time. After 12 weeks, patients commonly can transition to wearing a shoe. Inserts and ankle braces are often used. Physical therapy may be recommended. There are complications that relate to surgery in general. These include the risks associated with anesthesia, infection, damage to nerves and blood vessels, and bleeding or blood clots. Complications following flatfoot surgery may include wound breakdown or nonunion (incomplete healing of the bones). These complications often can be prevented with proper wound care and rehabilitation. Occasionally, patients may notice some discomfort due to prominent hardware. Removal of hardware can be done at a later time if this is an issue. The overall complication rates for flatfoot surgery are low. Overview
Children of many ages can have legs of unequal lengths. The medical diagnosis for this condition is called leg length discrepancy. The difference in length can be as small as one centimeter and as large as six centimeters or more. The greater the discrepancy, the more your child will have difficulty walking and maintaining proper posture. Significant differences in leg length can also cause functional scoliosis and problems with other parts of the legs and lower body. This makes leg length discrepancy treatment very important in order to maintain proper health and function of the child. The greater the difference in leg length, the higher the likelihood of necessary treatment.  Causes Some limb-length differences are caused by actual anatomic differences from one side to the other (referred to as structural causes). The femur is longer (or shorter) or the cartilage between the femur and tibia is thicker (or thinner) on one side. There could be actual deformities in one femur or hip joint contributing to leg length differences from side to side. Even a small structural difference can amount to significant changes in the anatomy of the limb. A past history of leg fracture, developmental hip dysplasia, slipped capital femoral epiphysis (SCFE), short neck of the femur, or coxa vara can also lead to placement of the femoral head in the hip socket that is offset. The end-result can be a limb-length difference and early degenerative arthritis of the hip. Symptoms The effects of limb length discrepancy vary from patient to patient, depending on the cause and size of the difference. Differences of 3 1/2 percent to 4 percent of the total length of the leg (about 4 cm or 1 2/3 inches in an average adult) may cause noticeable abnormalities when walking. These differences may require the patient to exert more effort to walk. There is controversy about the effect of limb length discrepancy on back pain. Some studies show that people with a limb length discrepancy have a greater incidence of low back pain and an increased susceptibility to injuries. Other studies do not support this finding. Diagnosis The most accurate method to identify leg (limb) length inequality (discrepancy) is through radiography. It?s also the best way to differentiate an anatomical from a functional limb length inequality. Radiography, A single exposure of the standing subject, imaging the entire lower extremity. Limitations are an inherent inaccuracy in patients with hip or knee flexion contracture and the technique is subject to a magnification error. Computed Tomography (CT-scan), It has no greater accuracy compared to the standard radiography. The increased cost for CT-scan may not be justified, unless a contracture of the knee or hip has been identified or radiation exposure must be minimized. However, radiography has to be performed by a specialist, takes more time and is costly. It should only be used when accuracy is critical. Therefore two general clinical methods were developed for assessing LLI. Direct methods involve measuring limb length with a tape measure between 2 defined points, in stand. Two common points are the anterior iliac spine and the medial malleolus or the anterior inferior iliac spine and lateral malleolus. Be careful, however, because there is a great deal of criticism and debate surrounds the accuracy of tape measure methods. If you choose for this method, keep following topics and possible errors in mind. Always use the mean of at least 2 or 3 measures. If possible, compare measures between 2 or more clinicians. Iliac asymmetries may mask or accentuate a limb length inequality. Unilateral deviations in the long axis of the lower limb (eg. Genu varum,?) may mask or accentuate a limb length inequality. Asymmetrical position of the umbilicus. Joint contractures. Indirect methods. Palpation of bony landmarks, most commonly the iliac crests or anterior iliac spines, in stand. These methods consist in detecting if bony landmarks are at (horizontal) level or if limb length inequality is present. Palpation and visual estimation of the iliac crest (or SIAS) in combination with the use of blocks or book pages of known thickness under the shorter limb to adjust the level of the iliac crests (or SIAS) appears to be the best (most accurate and precise) clinical method to asses limb inequality. You should keep in mind that asymmetric pelvic rotations in planes other than the frontal plane may be associated with limb length inequality. A review of the literature suggest, therefore, that the greater trochanter major and as many pelvic landmarks should be palpated and compared (left trochanter with right trochanter) when the block correction method is used. Non Surgical Treatment Treatment of leg length inequality involves many different approaches, such as orthotics, epiphysiodesis, shortening, and lengthening, which can be used alone or combined in an effort to achieve equalization of leg lengths. Leg length inequality of 2 cm or less is usually not a functional problem. Often, leg length can be equalized with a shoe lift, which usually corrects about two thirds of the leg length inequality. Up to 1 cm can be inserted in the shoe. For larger leg length inequalities, the shoe must be built up. This needs to be done for every shoe worn, thus limiting the type of shoe that the patient can wear. Leg length inequalities beyond 5 cm are difficult to treat with a shoe lift. The shoe looks unsightly, and often the patient complains of instability with such a large lift. A foot-in-foot prosthesis can be used for larger leg length inequalities. This is often done as a temporizing measure for young children with significant leg length inequalities. The prosthesis is bulky, and a fixed equinus contracture may result.  leg length discrepancy exercises Surgical Treatment Lengthening is usually done by corticotomy and gradual distraction. This technique can result in lengthenings of 25% or more, but typically lengthening of 15%, or about 6 cm, is recommended. The limits of lengthening depend on patient tolerance, bony consolidation, maintenance of range of motion, and stability of the joints above and below the lengthened limb. Numerous fixation devices are available, such as the ring fixator with fine wires, monolateral fixator with half pins, or a hybrid frame. The choice of fixation device depends on the desired goal. A monolateral device is easier to apply and better tolerated by the patient. The disadvantages of monolateral fixation devices include the limitation of the degree of angular correction that can concurrently be obtained; the cantilever effect on the pins, which may result in angular deformity, especially when lengthening the femur in large patients; and the difficulty in making adjustments without placing new pins. Monolateral fixators appear to have a similar success rate as circular fixators, especially with more modest lengthenings (20%). Overview
Heel pain is unlike most body aches and injuries because heels can?t be immobilized to rest and recover, at least without considerable inconvenience to the sufferer. Heels can?t be isolated and splinted either ,as body weight will continue to aggravate the condition with every step. Heel pain can be devastating if left untreated, eventually impairing the ability to walk comfortably-or at all. Most heel pain comes from tendon problems, though some types can come from bone issues as well. Causes There are several causes of heel pain. By far the most common cause in adults is a condition commonly known as plantar fasciitis. Other names occasionally used for the same condition are heel spurs, and policeman?s heel. Plantar means bottom of the foot, and fascia is the fibrous tissues that helps tether the heel bone (calcaneus) to the heads of the metatarsal bones found at the base of your toes The meaning of ?itis? is inflammation. However, inflammation does not have a large part to play in the pathology, it is more degenerative (wear & tear) so the preferred title is plantar fasciosis or plantar aponeurotic fasciosis. For simplicity sake, we will refer to this common cause of heel pain as plantar fasciitis in this manual. Symptoms See your doctor as soon as possible if you experience severe pain accompanied by swelling near your heel. There is numbness or tingling in the heel, as well as pain and fever. There is pain in your heel as well as fever. You are unable to walk normally. You cannot bend your foot downwards. You cannot stand with the backs of the feet raised (you cannot rise onto your toes). You should arrange to see a doctor if the heel pain has persisted for more than one week. There is still heel pain when you are not standing or walking. Diagnosis After you have described your foot symptoms, your doctor will want to know more details about your pain, your medical history and lifestyle, including. Whether your pain is worse at specific times of the day or after specific activities. Any recent injury to the area. Your medical and orthopedic history, especially any history of diabetes, arthritis or injury to your foot or leg. Your age and occupation. Your recreational activities, including sports and exercise programs. The type of shoes you usually wear, how well they fit, and how frequently you buy a new pair. Your doctor will examine you, including. An evaluation of your gait. While you are barefoot, your doctor will ask you to stand still and to walk in order to evaluate how your foot moves as you walk. An examination of your feet. Your doctor may compare your feet for any differences between them. Then your doctor may examine your painful foot for signs of tenderness, swelling, discoloration, muscle weakness and decreased range of motion. A neurological examination. The nerves and muscles may be evaluated by checking strength, sensation and reflexes. In addition to examining you, your health care professional may want to examine your shoes. Signs of excessive wear in certain parts of a shoe can provide valuable clues to problems in the way you walk and poor bone alignment. Depending on the results of your physical examination, you may need foot X-rays or other diagnostic tests. Non Surgical Treatment If you still have pain after several weeks, see your foot and ankle surgeon, who may add one or more of these treatment approaches, padding and strapping. Placing pads in the shoe softens the impact of walking. Strapping helps support the foot and reduce strain on the fascia. Orthotic devices. Custom orthotic devices that fit into your shoe help correct the underlying structural abnormalities causing the plantar fasciitis. Injection therapy. In some cases, corticosteroid injections are used to help reduce the inflammation and relieve pain. Removable walking cast. A removable walking cast may be used to keep your foot immobile for a few weeks to allow it to rest and heal. Night splint. Wearing a night splint allows you to maintain an extended stretch of the plantar fascia while sleeping. This may help reduce the morning pain experienced by some patients. Physical therapy. Exercises and other physical therapy measures may be used to help provide relief. Surgical Treatment With the advancements in technology and treatments, if you do need to have surgery for the heel, it is very minimal incision that?s done. And the nice thing is your recovery period is short and you should be able to bear weight right after the surgery. This means you can get back to your weekly routine in just a few weeks. Recovery is a lot different than it used to be and a lot of it is because of doing a minimal incision and decreasing trauma to soft tissues, as well as even the bone. So if you need surgery, then your recovery period is pretty quick. How do you treat heel pain? Prevention  A variety of steps can be taken to avoid heel pain and accompanying afflictions. Wear shoes that fit well-front, back, and sides-and have shock-absorbent soles, rigid shanks, and supportive heel counters. Wear the proper shoes for each activity. Do not wear shoes with excessive wear on heels or soles. Prepare properly before exercising. Warm up and do stretching exercises before and after running. Pace yourself when you participate in athletic activities. Don?t underestimate your body's need for rest and good nutrition. If obese, lose weight. Overview
 A neuroma is a thickening of nerve tissue that may develop in various parts of the body. The most common neuroma in the foot is a Morton?s neuroma, which occurs between the third and fourth toes. It is sometimes referred to as an intermetatarsal neuroma. ?Intermetatarsal? describes its location in the ball of the foot between the metatarsal bones. Neuromas may also occur in other locations in the foot. MortonThe thickening, or enlargement, of the nerve that defines a neuroma is the result of compression and irritation of the nerve. This compression creates enlargement of the nerve, eventually leading to permanent nerve damage. A neuroma is a thickening of nerve tissue that may develop in various parts of the body. The most common neuroma in the foot is a Morton?s neuroma, which occurs between the third and fourth toes. It is sometimes referred to as an intermetatarsal neuroma. ?Intermetatarsal? describes its location in the ball of the foot between the metatarsal bones. Neuromas may also occur in other locations in the foot. MortonThe thickening, or enlargement, of the nerve that defines a neuroma is the result of compression and irritation of the nerve. This compression creates enlargement of the nerve, eventually leading to permanent nerve damage.Causes Poorly fitted footwear can be a cause. Shoes that have a tight and narrow toe box can cause the never to become entrapped causing the pain. High heeled shoes abnormally place the metatarsals under extreme pressure which can cause Morton?s Neuroma. In cases of abnormal pronation, there can be significant motion between the 3rd and 4th metatarsals which can cause an irritation to the nerve that runs between them. This inflammation causes the pain. Symptoms The primary symptoms include sharp, shooting pain, numbness or paresthesia in the forefoot and extending distally into the toes, typically in the region of the third and fourth toes. Symptoms are aggravated with narrow toe box shoes or those with high heels. There is usually a reduction of symptoms when walking barefoot or wearing shoes with an appropriately wide toe box. Symptoms are also aggravated with shoes that are tied too tight. Diagnosis During the examination, your physician will feel for a palpable mass or a "click" between the bones. He or she will put pressure on the spaces between the toe bones to try to replicate the pain and look for calluses or evidence of stress fractures in the bones that might be the cause of the pain. Range of motion tests will rule out arthritis or joint inflammations. X-rays may be required to rule out a stress fracture or arthritis of the joints that join the toes to the foot. Non Surgical Treatment Initial treatment for Morton?s Neuroma may include non-prescription anti-inflammatory medications to reduce pain and swelling. These may consist of standard analgesics such as aspirin and ibuprofen (Advil, Motrin, others). Massaging the painful region three times daily with ice. Change of footwear. Avoid tight shoes, high heels or any footwear that seems to irritate the condition. Low heeled shoes with softer soles are preferable. Arch supports and foot pads to help reduce pressure on the nerve. In some cases, a physician may prescribe a customized shoe insert, molded to fit the contours of the patient?s foot. Reducing activities causing stress to the foot, including jogging, dancing, aerobic activity or any high impact movements of the foot. Injections of a corticosteroid medication to reduce the swelling and inflammation of the nerve and reduce pain. Occasionally other substances may be injected in order to ?ablate? the Neuroma. (The overuse of injected steroids is to be avoided however, as side effects, including weight gain and high blood pressure can result.)  Surgical Treatment For severe or persistent pain, you may need surgery to remove the neuroma. Once the nerve is gone, you permanently lose feeling in the affected area. One alternative to surgery is to undergo neurolysis injections. These use chemical agents to block pain signals. Another alternative is to take a prescription pain reliever that alleviates nerve pain. Prevention Ensuring that shoes are well fitted, low-heeled and with a wide toe area may help to prevent Morton's neuroma. There are actually two different kinds of leg length discrepancies, congenital and acquired. Congenital indicates that you are born with it. One leg is anatomically shorter compared to the other. Through developmental stages of aging, the human brain picks up on the gait pattern and identifies some variance. The human body usually adapts by tilting one shoulder over to the "short" side. A difference of less than a quarter inch is not blatantly excessive, demand Shoe Lifts to compensate and commonly does not have a serious effect over a lifetime.
 Leg length inequality goes typically undiagnosed on a daily basis, however this condition is very easily corrected, and can eradicate quite a few instances of back pain. Therapy for leg length inequality typically involves Shoe Lifts . Most are economical, normally costing less than twenty dollars, compared to a custom orthotic of $200 or more. Differences over a quarter inch can take their toll on the spine and should probably be compensated for with a heel lift. In some cases, the shortage can be so extreme that it requires a full lift to both the heel and sole of the shoe. Lumbar pain is easily the most common ailment afflicting people today. Over 80 million people are affected by back pain at some point in their life. It is a problem that costs employers millions yearly due to lost time and productivity. Fresh and more effective treatment solutions are continually sought after in the hope of minimizing the economical impact this issue causes.  People from all corners of the earth suffer from foot ache as a result of leg length discrepancy. In most of these situations Shoe Lifts are usually of beneficial. The lifts are capable of easing any discomfort in the feet. Shoe Lifts are recommended by many experienced orthopaedic orthopedists. In order to support the human body in a well-balanced manner, feet have a critical role to play. Inspite of that, it's often the most overlooked area of the body. Many people have flat-feet which means there is unequal force placed on the feet. This will cause other parts of the body such as knees, ankles and backs to be affected too. Shoe Lifts make sure that correct posture and balance are restored.  Overview A heel spur is a calcium deposit causing a bony protrusion on the underside of the heel bone. On an X-ray, a heel spur can extend forward by as much as a half-inch. Without visible X-ray evidence, the condition is sometimes known as "heel spur syndrome." Although heel spurs are often painless, they can cause heel pain. They are frequently associated with plantar fasciitis, a painful inflammation of the fibrous band of connective tissue (plantar fascia) that runs along the bottom of the foot and connects the heel bone to the ball of the foot. Treatments for heel spurs and associated conditions include exercise, custom-made orthotics, anti-inflammatory medications, and cortisone injections. If conservative treatments fail, surgery may be necessary. Causes A strong band of sinew (plantar fascia) stretches across the sole of the foot below the surface of the skin and is attached to a point in the middle of the under surface of the heel bone. With repeated activity on our feet, the plantar fascia can become tight and cause persistent traction (tugging) on its attachment point into the heel bone, and inflammation and pain may develop at this site. This painful condition is known as plantar fasciitis. Sometimes a ?spur? develops at the site of this traction on the bone and protrudes into the surrounding tissue. This is a heel spur.  Symptoms You may or may not experience any symptoms with your heel spurs. It is normally the irritation and inflammation felt in the tissues around your heel spur that cause discomfort. Heel pain is one of the first things you may notice, especially when pushing off the ball of your foot (stretches the plantar fascia). The pain can get worse over time and tends to be stronger in the morning, subsiding throughout the day; although it does return with increased activity. A sharp, poking pain in your heel that feels like you're stepping on a stone can often be felt while standing or walking. You will sometimes be able to feel a bump on the bottom of your heel, and occasionally bruising may appear. Diagnosis The diagnosis of heel pain and heel spurs is made by a through history of the course of the condition and by physical exam. Weight bearing x-rays are useful in determining if a heel spur is present and to rule out rare causes of heel pain such as a stress fracture of the heel bone, the presence of bone tumors or evidence of soft tissue damage caused by certain connective tissue disorders. Non Surgical Treatment Since heel spurs are not an indication of pain themselves unless fractured, treatment is usually aimed at the cause of the pain which in many cases is plantar fasciosis. Treatment of plantar fasciiosis includes; rest until the pain subsides, special stretching exercises and if required orthotics may be prescribed. Surgical Treatment Heel spur surgery should only be considered after less invasive treatment methods have been explored and ruled insufficient. The traditional surgical approach to treating heel spurs requires a scalpel cut to the bottom of the food which allows the surgeon to access the bone spur. Endoscopic plantar fasciotomies (EPF) involve one or two small incisions in the foot which allow the surgeon to access and operate on the bone spur endoscopically. Taking a surgical approach to heel spur treatment is a topic to explore with a foot and ankle specialist. Prevention A variety of steps can be taken to avoid heel pain and accompanying afflictions. Wear shoes that fit well-front, back, and sides-and have shock-absorbent soles, rigid shanks, and supportive heel counters. Wear the proper shoes for each activity. Do not wear shoes with excessive wear on heels or soles. Prepare properly before exercising. Warm up and do stretching exercises before and after running. Pace yourself when you participate in athletic activities. Don't underestimate your body's need for rest and good nutrition. If obese, lose weight.  Overview Heel spur is a thorn-like, bony protrusion of the heel bone, which can become inflamed through irritation, thus causing pain. A heel spur forms at the tendon attachments on the muscles of the heel bone as a result of micro-injuries to the tissue caused by overstraining. As part of the healing process for these micro-injuries, the body stores bone material in the tendon attachments as a repair mechanism. Heel spurs can develop over a very long period without causing major complaints. However, irritation of the area surrounding the ossified tendon attachment can cause inflammations. Left untreated, the inflammations can in turn lead to increased ossification and thus to permanent degradation with a risk of chronic manifestation. The normal rolling procedure that we all use when walking is then frequently no longer possible. Causes At the onset of this condition, pain and swelling become present, with discomfort particularly noted as pushing off with the toes occurs during walking. This movement of the foot stretches the fascia that is already irritated and inflamed. If this condition is allowed to continue, pain is noticed around the heel region because of the newly formed bone, in response to the stress. This results in the development of the heel spur. It is common among athletes and others who run and jump a significant amount. 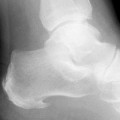 Symptoms Heel spurs often cause no symptoms. But heel spurs can be associated with intermittent or chronic pain, especially while walking, jogging, or running, if inflammation develops at the point of the spur formation. In general, the cause of the pain is not the heel spur itself but the soft-tissue injury associated with it. Many people describe the pain of heel spurs and plantar fasciitis as a knife or pin sticking into the bottom of their feet when they first stand up in the morning, a pain that later turns into a dull ache. They often complain that the sharp pain returns after they stand up after sitting for a prolonged period of time. Diagnosis A heel spur is often seen on X-ray as a bony protrusion, which can vary in size. However, because a Heel Spur only indicates increased load on the plantar fascia, and not pain, an ultra sound may be required to assess other actual cause of the heel pain such and may include checking to see if the plantar fascia is inflamed or degenerated. Non Surgical Treatment Heel spurs and plantar fascitis (inflammation of the plantar fascia) are usually controlled with conservative treatment. Early intervention includes stretching the calf muscles while avoiding reinjury to the plantar fascia. Decreasing or changing activities, losing excess weight, and improving the fit of shoes are all important measures to decrease foot pain. Modification of footwear includes well-padded shoes with a raised heel and better arch support. Shoe inserts recommended by a healthcare professional are often very helpful when used with exercises to increase the strength of the foot muscles and arch. The inserts prevent excessive pronation and continued tearing of the plantar fascia. Surgical Treatment More than 90 percent of people get better with nonsurgical treatments. If conservative treatment fails to treat symptoms of heel spurs after a period of 9 to 12 months, surgery may be necessary to relieve pain and restore mobility. Surgical techniques include release of the plantar fascia, removal of a spur. Pre-surgical tests or exams are required to identify optimal candidates, and it's important to observe post-surgical recommendations concerning rest, ice, compression, elevation of the foot, and when to place weight on the operated foot. In some cases, it may be necessary for patients to use bandages, splints, casts, surgical shoes, crutches, or canes after surgery. Possible complications of heel surgery include nerve pain, recurrent heel pain, permanent numbness of the area, infection, and scarring. In addition, with plantar fascia release, there is risk of instability, foot cramps, stress fracture, and tendinitis. Prevention Walk around before you buy shoes. Before you purchase your shoes, do the following. Re-lace the shoes if you're trying on athletic shoes. Start at the farthest eyelets and apply even pressure to the laces as you come closer to the tongue of the shoe. Make sure that you can wiggle your toes freely inside of the shoe. Also, make sure that you have at enough space between your tallest toe and the end of the shoe. You should have room equal to about the width of your thumb in the tip of your shoe. Walk around to make sure that the shoe has a firm grip on your heel without sliding up and down. Walk or run a few steps to make sure your shoes are comfortable. Shoes that fit properly require no break-in period. Overview
Retrocalcaneal bursitis is sometimes difficult to differentiate from Achilles tendinitis, at least symptomatically. Both are most uncomfortable during the push-off phase of gait, are most severely painful in the morning and with walking after sitting for a period of time, and generally worsen with activity. Most practitioners make the distinction between the two simply on the basis of location of pain and tenderness. Generally, Achilles tendinitis is felt an inch or two higher than this form of bursitis. Causes Bursitis of the Achilles tendon is caused by the irritation and inflammation of the retrocalcaneal bursa, a small fluid-filled sac located in the back of the ankle that acts as a cushion and lubricant for the ankle joint. Possible causes of Achilles tendon bursitis include aging, Factors related to the aging process, including the onset of rheumatoid arthritis and gout, can deteriorate the bursa. Overuse of ankle. Excessive walking, uphill running, jumping, and other aggressive exercise regimens, especially without proper conditioning, can cause irritation to the bursa. Trauma. Sudden injury to the ankle joint, or trauma caused by rigid or improperly fitted shoes, can increase the chances of developing bursitis. Symptoms Medical experts strongly recommend that you consult a doctor if you have any of the symptoms below. Disabling joint pain that prevents you from doing your daily activities. Pain that lasts for more than two weeks. Excessive swelling, redness, bruising or a rash around the painful joint. Sharp or shooting pain, especially when you exercise or do something more strenuous. A fever. Any of the above could be a sign of infection, a condition such as arthritis or a more serious injury such as a tendon tear that may require medical attention. Diagnosis Your health care provider will take a history to find out if you have symptoms of retrocalcaneal bursitis. Examining your ankle can find the location of the pain. The physician will look for tenderness and redness in the back of the heel. The pain may be worse when the doctor bends the ankle upward (dorsiflex). Or, the pain may be worse when you rise on your toes. You will not usually need imaging studies such as x-ray and MRI at first. If the first treatment does not improve the symptoms, your health care provider may recommend these tests. MRI may show inflammation. Non Surgical Treatment In addition to R.I.C.E., there are a number of other treatments to reduce swelling and any associated pain or discomfort due to heel bursitis. Orthotics or change of footwear. Wearing an orthotic device such as a heel insert can encourage better mechanics in the foot and reduce irritation of the retrocalcaneal bursa. Some people do not need special orthotics but simply need to stop wearing shoes with rigid heel and ankle construction and instead wear more supportive, comfortable shoes. Shoes with an "Achilles notch," a groove in the collar at the back of the shoe to protect the Achilles tendon, can be particularly helpful. (Almost all running shoes are designed with an Achilles notch.) Stretching and physical therapy. Stretching the Achilles tendon often helps alleviate pain. Once the pain is resolved it is important for the patient to continue a regular stretching program. Regular stretching reduces the chance of recurrence. Surgical Treatment Bursectomy is a surgical procedure used to remove an inflamed or infected bursa, which is a fluid-filled sac that reduces friction between tissues of the body. Because retrocalcaneal bursitis can cause chronic inflammation, pain and discomfort, bursectomy may be used as a treatment for the condition when it is persistent and cannot be relived with other treatments. During this procedure, a surgeon makes small incisions so that a camera may be inserted into the joint. This camera is called an arthroscope. Another small incision is made so that surgical instruments can be inserted to remove the inflamed bursa.  Overview OverviewEssentially, there's one consistent type of hammertoe, the condition in which your toes are contracted into a hammer or upside-down "V" shape. However, depending on its severity, hammertoe is characterized into two forms. Flexible hammertoe is hammertoe in which the joints of the toes are still moveable or flexible and can be treated with nonsurgical therapies. Rigid hammertoe is the more serious condition in which the joints' muscles and tendons have lost any flexibility and the contraction cannot be corrected by nonsurgical means. As a result, surgery is generally required to deal with the problem. This is why it's important to consult a physician as soon as the problem is recognized for the possibility of successful nonsurgical treatment. Causes Hammertoe commonly develops because of structural changes that take place over time in the muscles and tendons that bend the toes. People with certain medical conditions, such as diabetes, are at risk for developing hammertoe. It can be an inherited condition for some people. Other causes include trauma and wearing shoes that are too tight, narrow, or have high heels. The toe next to the big toe (second toe) is most frequently affected by hammertoe.  Symptoms SymptomsThe most obvious symptom of hammer, claw or mallet toe is the abnormal toe position. This is usually combined with pain: the abnormal foot position leads to excessive friction on the toe as it rubs against any footwear which hammertoe can be extremely painful. Corns & Calluses: repeated friction can result in the formation of a foot corn or callus on top of the toes. Stiffness, the joints become increasingly stiff. In the early stages, the toes can usually be straightened out passively using your hands, but if allowed to progress, the stiffness may be permanent. Diagnosis Hammertoes are progressive, they don?t go away by themselves and usually they will get worse over time. However, not all cases are alike, some hammertoes progress more rapidly than others. Once your foot and ankle surgeon has evaluated your hammertoes, a treatment plan can be developed that is suited to your needs. Non Surgical Treatment Wear wide shoes with plenty of room in the toes and resilient soles. Avoid wearing shoes with pointed toes. Commercially available felt pads or cushions may ease pressure from the shoe on the toe. Toe caps (small, padded sleeves that fit around the tip of the toe) may relieve the pain of hammer toe. Do toe exercises, to help toe muscles become stronger and more flexible. Arch supports or an orthotic shoe insert prescribed by your doctor or podiatrist may help to redistribute weight on the foot. These devices do not cure the problem but may ease the symptoms of either hammer toe or mallet toe. Surgical Treatment If pinning the toe is not required during the procedure, then the surgery could be preformed in the doctor's office under a local anesthesia. Some patients prefer the comfort of sedation during the surgery and if this is the case or if a pin must be placed, then the surgery could be preformed in an outpatient surgery center. Overview
Pronation describes the natural process of the inward rolling of your foot when the outer edge of your heel strikes the ground and your foot flattens out. Excess pronation, known as flat foot, can result in flattened arches and overstretched foot muscles. Advanced conditions may affect your hips, knees, ankle, back and foot functioning. Use natural techniques to stretch and strengthen your muscles in order to help pronation.  Causes It is important to identify the cause of overpronation in order to determine the best treatment methods to adopt. Not all treatments and preventative measures will work equally well for everyone, and there may be a little trial and error involved to get the best treatment. A trip to a podiatrist or a sports therapist will help you to establish the cause of overpronation, and they will be able to tell you the best treatments based on your specific degree of overpronation and the cause. Overpronation has many causes, with the most common reasons for excessive pronation listed, low arches, flexible flat feet, fallen arches, gait abnormalities, abnormal bone structure, abnormal musculature, bunions, corns and calluses. Symptoms Common conditions seen with overpronation include heel pain or plantar fasciitis, achilles tendonopathy, hallus valgus and or bunions, patellofemoral pain syndrome, Iliotibial band pain syndrome, low back pain, shin splints, stress fractures in the foot or lower leg. Diagnosis To easily get an idea of whether a person overpronates, look at the position and condition of certain structures in the feet and ankles when he/she stands still. When performing weight-bearing activities like walking or running, muscles and other soft tissue structures work to control gravity's effect and ground reaction forces to the joints. If the muscles of the leg, pelvis, and feet are working correctly, then the joints in these areas such as the knees, hips, and ankles will experience less stress. However, if the muscles and other soft tissues are not working efficiently, then structural changes and clues in the feet are visible and indicate habitual overpronation.  Non Surgical Treatment Supportive orthotics in the shoe is a method commonly implemented to treat many common running injuries associated with pronation. An advantage of orthotics is that they often allow the sufferer to continue to participate in athletic activity and avoid other treatment options that could be potentially costly and time consuming. Seventy-five percent of injured runners are successfully treated with the prescription of orthoses. Orthotics are the most effective treatment for symptoms that develop from unusual biomechanics within the body such as overpronation, resulting in either great improvement or complete healing of the injury in about half the cases. Prevention Duck stance: Stand with your heels together and feet turned out. Tighten the buttock muscles, slightly tilt your pelvis forwards and try to rotate your legs outwards. You should feel your arches rising while you do this exercise. Calf stretch:Stand facing a wall and place hands on it for support. Lean forwards until stretch is felt in the calves. Hold for 30 seconds. Bend at knees and hold for a further 30 seconds. Repeat 5 times. Golf ball:While drawing your toes upwards towards your shins, roll a golf ball under the foot between 30 and 60 seconds. If you find a painful point, keep rolling the ball on that spot for 10 seconds. Big toe push: Stand with your ankles in a neutral position (without rolling the foot inwards). Push down with your big toe but do not let the ankle roll inwards or the arch collapse. Hold for 5 seconds. Repeat 10 times. Build up to longer times and fewer repetitions. Ankle strengthener: Place a ball between your foot and a wall. Sitting down and keeping your toes pointed upwards, press the outside of the foot against the ball, as though pushing it into the wall. Hold for 5 seconds and repeat 10 times. Arch strengthener: Stand on one foot on the floor. The movements needed to remain balanced will strengthen the arch. When you are able to balance for 30 seconds, start doing this exercise using a wobble board. |
|
